What is Gastric Bypass Surgery?
Gastric bypass surgery, also known as Roux-en-Y gastric bypass (RGB), is the most commonly performed weight-loss surgery procedure and is considered the gold standard in bariatric surgery.
This transformative procedure combines two powerful approaches to help patients achieve significant and lasting weight loss.
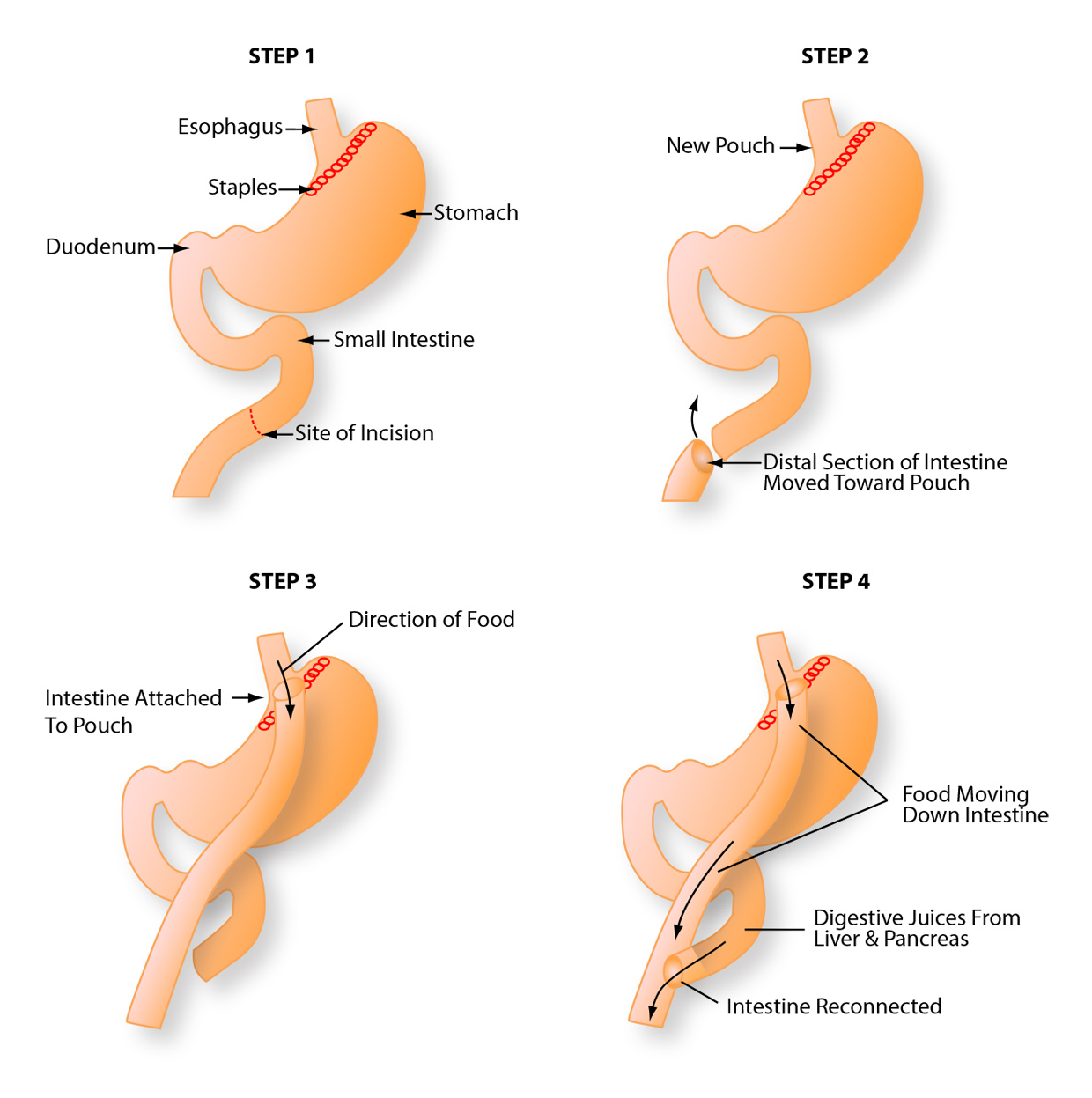
First, your surgeon creates a small pouch at the top of your stomach using surgical staples, dramatically reducing the amount of food your stomach can hold at one time (typically to about the size of an egg). Next, a Y-shaped section of your small intestine is carefully attached to this newly created pouch, allowing food to bypass the upper portion of your stomach and the first section of your small intestine (the duodenum).
This dual mechanism works in two important ways: it restricts the volume of food you can consume at one time, and it reduces the amount of calories and nutrients your digestive system absorbs from the food you eat. The result is a powerful combination that helps patients achieve substantial weight loss. At MemorialCare, gastric bypass surgery can be performed using advanced robotic surgical systems, which provide our surgeons with enhanced visualization, precision, and control while requiring only small incisions of 1-2 cm.
Gastric bypass surgery is primarily designed to treat severe obesity and its associated health conditions. You may be a candidate for this procedure if you have a body mass index (BMI) of 40 or higher, or a BMI of 35 or higher with serious obesity-related health problems.
The procedure has been shown to effectively treat or significantly improve numerous obesity-related conditions, including:
- Type 2 Diabetes: Weight-loss surgery can lead to remission or significant improvement of type 2 diabetes in many patients, often reducing or eliminating the need for diabetes medications.
- Cardiovascular Disease: Gastric bypass helps reduce risk factors for heart disease, including high blood pressure, high cholesterol, and excess weight on the heart.
- Sleep Apnea: Many patients experience complete resolution or significant improvement of obstructive sleep apnea after substantial weight loss.
- Joint Pain and Osteoarthritis: Reducing excess weight relieves pressure on weight-bearing joints, particularly knees, hips, and ankles.
- Fatty Liver Disease: The procedure can help reverse non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH).
- Gastroesophageal Reflux Disease (GERD): Many patients see improvement in acid reflux symptoms following gastric bypass surgery.
- Metabolic Syndrome: The combination of conditions, including high blood pressure, high blood sugar, excess body fat, and abnormal cholesterol levels, often improves dramatically.
Beyond physical health improvements, gastric bypass surgery can also lead to enhanced quality of life, increased mobility, improved self-esteem, and better emotional well-being. Many of our patients at the MemorialCare Surgical Weight Loss Center report feeling more confident, energetic, and able to participate in activities they previously found challenging.
Gastric bypass surgery is not for everyone, and determining candidacy requires careful evaluation by our multidisciplinary team. Generally, you may be a candidate if you:
- Have a BMI of 40 or higher (approximately 100 pounds or more overweight for men, or 80 pounds or more for women)
- Have a BMI of 35 or higher with at least one serious obesity-related health condition, such as type 2 diabetes, sleep apnea, or heart disease
- Have attempted to lose weight through diet and exercise without long-term success
- Are committed to making permanent lifestyle changes, including dietary modifications and regular exercise
- Understand the risks and benefits of the procedure
- Are psychologically prepared for the challenges and changes that come with bariatric surgery
- Do not have medical conditions that make surgery too risky
At MemorialCare, our comprehensive evaluation process includes consultations with bariatric surgeons, nutritionists, psychologists, and other specialists to ensure you're fully prepared for this life-changing journey. We want to set you up for long-term success, which requires not only the surgery itself, but also your full commitment to behavioral changes and medical follow-up for life.
Procedure Details
Preparing for gastric bypass surgery is a comprehensive process that typically takes several weeks to months. At the MemorialCare Surgical Weight Loss Center, we guide you through each step to ensure you're physically and mentally ready for surgery and the lifestyle changes that follow.
Medical Evaluation: You'll undergo a thorough medical assessment, including blood work, imaging studies, and possibly additional tests such as an EKG, chest X-ray, or sleep study. Your surgeon will review your complete medical history and current medications.
Nutritional Counseling: Our registered dietitians will work with you to establish healthy eating habits before surgery. You'll learn about proper nutrition, portion control, and the specific dietary requirements you'll need to follow after your procedure. Most patients will follow a preoperative diet for 2-4 weeks before surgery, which typically includes a low-calorie, high-protein liquid diet designed to reduce liver size and make surgery safer.
Psychological Assessment: Meeting with a psychologist helps ensure you're emotionally prepared for the significant lifestyle changes ahead. This evaluation also identifies any mental health concerns that should be addressed before surgery to support your long-term success.
Education Sessions: You'll attend educational seminars where you'll learn about the surgery itself, what to expect during recovery, potential complications, and the lifestyle modifications necessary for success.
Lifestyle Modifications: In the weeks leading up to surgery, you'll be asked to quit smoking (if applicable), limit alcohol consumption, and begin incorporating light physical activity into your daily routine. These changes help reduce surgical risks and establish healthy habits for after surgery.
Insurance Authorization: Our dedicated insurance specialists will work with your insurance provider to obtain necessary pre-authorizations. Many insurance companies cover weight-loss surgery when medical criteria are met, as explained in the American Society for Metabolic and Bariatric Surgery guidelines.
The weeks before surgery are also the perfect time to prepare your home for recovery. Stock your kitchen with approved foods, arrange for help during the first week or two at home, and organize a comfortable recovery space. This preparation period is essential for achieving the best possible outcomes.
At MemorialCare, gastric bypass surgery is typically performed using minimally invasive laparoscopic or robotic-assisted techniques, which offer significant advantages over traditional open surgery. The procedure usually takes 2-4 hours to complete and is performed under general anesthesia.
Step 1: Creating the Gastric Pouch Your surgeon begins by using surgical staples to divide your stomach, creating a small pouch at the top that's roughly the size of an egg (holding only about 1 ounce or 30 milliliters). This new, smaller stomach pouch will be the only part of your stomach that receives food, immediately limiting how much you can eat at one time.
Step 2: Dividing the Small Intestine The small intestine is then carefully divided a short distance below the main stomach. The lower section of the divided small intestine (the Roux limb) is brought up and connected to the newly created stomach pouch.
Step 3: Creating the Y Connection The upper portion of the small intestine, which is still connected to the bypassed portion of your stomach, is reconnected to the small intestine further down, creating a distinctive Y shape (hence "Roux-en-Y"). This configuration allows digestive juices from the bypassed stomach, pancreas, and liver to mix with food further along in the intestine.
Robotic and Laparoscopic Advantages
When performed robotically or laparoscopically, your surgeon makes only four to six small incisions (typically 1-2 cm each) in your abdomen. Tiny surgical instruments and a high-definition camera are inserted through these incisions, allowing your surgeon to operate with enhanced precision, improved visualization, and greater dexterity. This minimally invasive approach typically results in less pain, fewer complications, shorter hospital stays, faster recovery, and minimal scarring compared to traditional open surgery.
Throughout the procedure, our experienced surgical team, including specialized bariatric nurses and anesthesiologists, monitors you closely to ensure your safety and comfort. The MemorialCare Surgical Weight Loss Center team has performed thousands of these procedures and is led by bariatric surgery pioneers with extensive expertise in advanced surgical techniques.
Recovery from gastric bypass surgery is a gradual process that varies from patient to patient, but most people can expect to follow a similar timeline. Understanding what to expect helps you prepare mentally and physically for your postoperative journey.
In the Hospital (1-3 days): Most patients stay in the hospital for 1-3 days after surgery. During this time, our nursing staff will help you with pain management, encourage you to begin walking (usually within a few hours of surgery), and start you on a clear liquid diet. Walking is crucial for preventing blood clots and promoting healing. You'll receive instructions on caring for your incisions and recognizing signs of potential complications before you're discharged.
First Two Weeks at Home: The initial recovery period requires rest and adherence to your post-operative dietary guidelines. You'll continue with clear liquids for the first few days, then gradually progress to full liquids. Pain and discomfort are typically manageable with prescribed medications. Most patients can resume light activities and short walks, but should avoid heavy lifting, strenuous exercise, and driving while taking pain medication.
Weeks 2-4: As you continue healing, you'll transition through different diet stages under the guidance of your MemorialCare dietitian. This typically progresses from pureed foods to soft foods. Many patients begin to feel significantly better during this period and can return to work if their job doesn't involve heavy physical labor.
Weeks 4-8: By the fourth week, most patients can gradually introduce regular foods back into their diet, following the guidelines provided by the nutrition team. You'll be eating small, frequent meals and focusing on protein-rich foods. Exercise becomes increasingly important during this phase, and you should be establishing a regular physical activity routine.
Long-Term Recovery: The first 6-12 months after surgery represent a critical period for weight loss and habit formation. During this time, you'll have regular follow-up appointments with your surgical team, attend support groups, and work closely with our nutritionists to ensure you're meeting your nutritional needs and weight loss goals. Most patients lose 5-6 pounds per week during the first six weeks, with continued steady weight loss of 1-2 pounds per week for several months thereafter. Patients typically lose approximately two-thirds of their excess weight within the first two years.
It's important to remember that gastric bypass is a tool, not a cure. Long-term success requires permanent lifestyle changes, including mindful eating, regular exercise, vitamin supplementation, and ongoing medical follow-up. The comprehensive support system at the MemorialCare Surgical Weight Loss Center, including our experienced surgeons, nutritionists, psychologists, and counselors, is here to support you throughout your entire weight-loss journey.
Risks & Benefits
Gastric bypass surgery offers life-changing benefits that extend far beyond weight loss. When patients commit to the necessary lifestyle changes and follow their postoperative care plans, the results can be truly transformative.
Significant and Sustained Weight Loss: Gastric bypass operations that combine restriction and malabsorption typically result in more weight loss than procedures that only restrict food intake. Patients generally lose approximately two-thirds to 80% of their excess weight within the first two years. This substantial weight reduction dramatically improves overall health and quality of life.
Resolution or Improvement of Comorbidities: One of the most remarkable benefits of gastric bypass is its effect on obesity-related health conditions. Studies have shown that weight-loss surgery can potentially reverse or significantly improve type 2 diabetes in up to 80% of patients, often within weeks of surgery and before significant weight loss occurs. The procedure has similar positive effects on high blood pressure, high cholesterol, sleep apnea, and fatty liver disease. Many patients are able to reduce or eliminate medications for these conditions under their doctor's supervision.
Enhanced Quality of Life: Beyond the medical improvements, patients report profound increases in quality of life. Increased mobility makes everyday activities easier and more enjoyable. Many patients find they can participate in activities with family and friends that were previously impossible, from playing with grandchildren to traveling comfortably. Physical limitations that once prevented them from living fully are significantly reduced or eliminated.
Psychological and Social Benefits: As patients lose weight and regain health, they often experience increased self-esteem, improved body image, and enhanced emotional well-being. Social interactions become easier and more enjoyable. Many patients report feeling more confident in professional and personal settings. The psychological benefits of successful weight loss can be just as significant as the physical improvements.
Extended Life Expectancy: Research indicates that significant weight loss achieved through bariatric surgery may increase life expectancy by reducing the risk of premature death from obesity-related conditions such as heart disease, stroke, and certain cancers, according to studies published by the National Institutes of Health.
Improved Metabolic Function: Gastric bypass surgery affects gut hormones and metabolism in ways that go beyond simple calorie restriction. These metabolic changes can lead to improved insulin sensitivity, better blood sugar control, and reduced hunger signals, all of which support long-term weight maintenance.
At MemorialCare, we've witnessed countless success stories from patients who have transformed their lives through gastric bypass surgery. Our multidisciplinary team is committed to helping you achieve and maintain these life-changing benefits through comprehensive preoperative preparation, expert surgical care, and ongoing postoperative support.
While gastric bypass surgery offers significant benefits, it's important to understand potential side effects so you can make an informed decision and be prepared for what to expect.
Dumping Syndrome: This is one of the most common side effects unique to gastric bypass. Dumping syndrome occurs when food, especially foods high in sugar or fat, moves too quickly from your stomach pouch into your small intestine. Symptoms can include nausea, vomiting, diarrhea, dizziness, rapid heart rate, cold sweats, and cramping. While uncomfortable, dumping syndrome typically subsides within 30-60 minutes and can often be prevented by avoiding high-sugar and high-fat foods, eating slowly, and not drinking fluids with meals.
Nutritional Deficiencies: Because gastric bypass causes food to bypass the duodenum (where most iron and calcium are absorbed), nutritional deficiencies are common without proper supplementation. You'll need to take vitamin and mineral supplements for life, including a multivitamin, calcium with vitamin D, vitamin B12, and iron. Your healthcare team will monitor your nutrient levels through regular blood tests and adjust your supplements as needed.
Nausea and Vomiting: These are common in the first few months after surgery, particularly when patients eat too quickly, don't chew food thoroughly, or eat too much at once. Following dietary guidelines and eating mindfully usually prevents these issues.
Gastrointestinal Discomfort: Some patients experience increased gas, bloating, or changes in bowel habits as their digestive system adjusts to the new anatomy. These symptoms typically improve over time as your body adapts.
Food Intolerances: After surgery, you may find that certain foods that you previously tolerated well now cause discomfort. Common problem foods include red meat, bread, pasta, and fibrous vegetables. Food tolerances often improve over time, but some remain permanent.
Hair Thinning: Temporary hair loss can occur 3-6 months after surgery due to the stress of surgery, rapid weight loss, and potential protein or nutrient deficiencies. This is usually temporary, and hair typically regrows once weight stabilizes and nutritional status improves.
Excess Skin: Significant weight loss can result in excess, loose skin, particularly on the abdomen, arms, thighs, and breasts. Some patients choose to have plastic surgery procedures to remove excess skin once their weight has stabilized.
Gallstones: Rapid weight loss increases the risk of developing gallstones. Your surgeon may prescribe medication to reduce this risk during the period of rapid weight loss.
Most side effects can be minimized or managed with proper education, adherence to dietary guidelines, vitamin supplementation, and regular follow-up care. Your MemorialCare care team will prepare you for these possibilities and provide strategies to manage them effectively.
As with any major surgery, gastric bypass carries potential risks and complications. While serious complications are rare, particularly when surgery is performed by experienced surgeons at accredited centers like MemorialCare, it's essential to understand these risks.
Surgical Risks (Short-term):
Bleeding: Though uncommon, internal bleeding can occur during or after surgery and may require blood transfusion or additional surgery.
Infection: Surgical site infections or internal infections can develop. These are typically treated with antibiotics; however, additional procedures may be necessary in some cases.
Blood Clots: Blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism) are serious but rare complications. Early walking after surgery and the use of blood-thinning medications help reduce this risk.
Adverse Reactions to Anesthesia: Some patients may have unexpected reactions to anesthesia, though this is uncommon with modern anesthetic techniques.
Leakage: A leak where the stomach pouch connects to the intestine is a serious complication that occurs in approximately 1-3% of patients. This may require additional surgery or a prolonged hospital stay.
Long-term Complications:
Internal Hernias: Part of the intestine can protrude through openings created during surgery, potentially requiring surgical repair.
Bowel Obstruction: Scar tissue or internal hernias can cause bowel blockage, which may need surgical intervention.
Marginal Ulcers: Ulcers can develop at the connection between the stomach pouch and intestine, particularly in patients who smoke, take NSAIDs, or have H. pylori infection.
Strictures: The connection between the stomach pouch and small intestine may narrow over time, causing difficulty swallowing or vomiting. This can usually be treated with endoscopic dilation.
Pouch Stretching: The stomach pouch can gradually enlarge if you consistently overeat, potentially leading to weight regain. Following portion size guidelines is essential to prevent this.
Hypoglycemia: Some patients develop low blood sugar episodes (reactive hypoglycemia) months or years after surgery, particularly after consuming high-sugar foods.
Malnutrition: Without proper vitamin supplementation and adequate protein intake, serious nutritional deficiencies can develop, negatively impacting your health and quality of life.
Weight Regain: While gastric bypass is highly effective, 20-30% of patients may regain some weight over time if they don't maintain lifestyle changes. However, even with some weight regain, most patients maintain significant weight loss compared to their pre-surgery weight.
At MemorialCare, we minimize these risks through careful patient selection, comprehensive pre-operative preparation, advanced surgical techniques, and meticulous post-operative care. Our surgical team has extensive experience performing these procedures, and our center is accredited by the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery, demonstrating our commitment to safety and quality.
If complications arise, our team is well-equipped to manage them effectively. We encourage patients to maintain regular follow-up appointments and to contact us immediately if they experience concerning symptoms. Should you require revision weight-loss surgery in the future, our experienced team will be happy to discuss your options with you.
Gastric bypass surgery has an excellent track record when patients commit to the necessary lifestyle changes and follow their postoperative care plans. Success is measured not just in pounds lost, but in improved health, enhanced quality of life, and sustained weight maintenance.
Weight Loss Success: Most patients achieve significant weight loss, with studies showing that patients typically lose 60-80% of their excess body weight within the first two years after surgery. For example, a patient who is 100 pounds overweight can expect to lose approximately 60 to 80 pounds. Many patients experience a loss of 5-6 pounds per week during the first six weeks after surgery, with continued weight loss of 1-2 pounds per week for several months thereafter. Weight loss typically peaks around 12 to 18 months post-surgery, after which weight stabilizes.
Health Improvement Success: The success of gastric bypass in resolving obesity-related health conditions is remarkable. Research shows:
- Type 2 diabetes remission in 75-80% of patients
- Significant improvement or resolution of high blood pressure in 70-80% of patients
- Resolution of sleep apnea in 80-85% of patients
- Improvement in high cholesterol in 70% of patients
- Significant reduction in joint pain and improved mobility in the majority of patients
Long-term Success Factors: The most successful patients share common characteristics:
- They attend all follow-up appointments and support groups
- They strictly follow dietary guidelines and take prescribed vitamin supplements
- They incorporate regular physical activity into their daily routines
- They seek support when facing challenges
- They view surgery as a tool rather than a complete solution
The MemorialCare Advantage
At the MemorialCare Surgical Weight Loss Center at Orange Coast Medical Center, our success rates are among the best in the region. Our surgical team has performed more than 12,500 weight-loss surgeries. We are an Accredited Metabolic and Bariatric Surgical Center by the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery, demonstrating our commitment to providing high-quality care and optimal patient outcomes.
Our comprehensive approach encompasses not only expert surgical care but also ongoing support from nutritionists, psychologists, counselors, and support groups. This multidisciplinary team approach significantly enhances success rates by addressing all aspects of your weight-loss journey.
While individual results vary, the overwhelming majority of our patients report that gastric bypass surgery was a life-changing decision that restored their health and quality of life. As one of our patients shared, "I'm doing better now in my 70s than I was in my 50s. They gave me what I needed to be successful, and I continue to attend the support groups to this day."
Your Next Steps with MemorialCare
Every patient's journey is unique, and your MemorialCare care team will personalize your treatment plan to meet your individual needs and goals. We'll guide you through every step of the process, from initial consultation through long-term follow-up, ensuring you understand the risks and benefits before proceeding. Our comprehensive support system, including experienced surgeons, dedicated nutritionists, psychologists, and support groups, is here to help you achieve lasting success.
Ready to take the first step toward a healthier life? Contact the MemorialCare Surgical Weight Loss Center at (714) 378-7622 or schedule a consultation and learn whether gastric bypass surgery is right for you. Our compassionate team is here to answer your questions and support you on your weight-loss journey.
FAQs about Gastric Bypass Surgery
Pain levels vary from person to person, but most patients report that their pain is manageable with prescribed medications. Because gastric bypass at MemorialCare is typically performed using minimally invasive laparoscopic or robotic techniques, post-operative pain is generally less severe than with traditional open surgery. You'll likely experience some discomfort around your incision sites and may feel soreness in your abdomen and shoulders (from the gas used during surgery) for the first few days. Most patients experience a significant decrease in pain within the first week, and many are able to discontinue their pain medication within 7-10 days. Walking regularly after surgery can actually help reduce pain and speed recovery.
Most gastric bypass patients stay in the hospital for 1 to 3 days after surgery. The exact length depends on your individual recovery and whether any complications arise. During your hospital stay, our medical team will closely monitor you, help manage your pain, encourage you to walk, and initiate your liquid diet. You'll be discharged once you can tolerate liquids, your pain is well-controlled with oral medications, and you're able to walk independently. Before leaving, you'll receive detailed instructions for home care and follow-up appointments.
Yes, following a specific dietary progression is crucial for proper healing and long-term success. Your MemorialCare dietitian will guide you through several phases: Stage 1 (Days 1-7) involves clear liquids only. Stage 2 (Weeks 2-3) progresses to full liquids, including protein shakes. Stage 3 (Week 4) introduces pureed foods. Stage 4 (Weeks 5-8) includes soft foods, and finally, you'll transition to regular foods, though you'll need to eat small portions (2-4 ounces per meal) and focus on protein-rich choices. You'll need to avoid high-sugar and high-fat foods to prevent dumping syndrome. Eating slowly, chewing thoroughly, and avoiding drinking liquids with meals are lifetime habits you'll need to develop. Your nutrition team will provide detailed guidelines and support throughout each stage.
Dietary Guidelines
Many insurance companies do cover gastric bypass surgery when specific medical criteria are met. Most insurers require documentation that you have a BMI of 40 or higher, or a BMI of 35 or higher with serious obesity-related health conditions such as type 2 diabetes, heart disease, or sleep apnea. You'll typically need to show evidence of previous weight-loss attempts and may be required to complete a medically supervised diet program before surgery. The knowledgeable insurance specialists at the MemorialCare Surgical Weight Loss Center will work directly with you and your insurance provider to verify coverage, obtain necessary pre-authorizations, and help make financial arrangements. We accept most major HMO, PPO, and EPO health plans, as well as Medicare and private insurance. For more information about accepted health plans, visit our website or contact our center directly.
Yes, many women successfully become pregnant after gastric bypass surgery, and weight loss can actually improve fertility. However, it's strongly recommended that you wait 12-18 months after surgery before trying to conceive. This waiting period allows your weight to stabilize and ensures your nutritional status is optimized before pregnancy. During pregnancy after gastric bypass, you'll need close monitoring by both your obstetrician and bariatric team to ensure adequate nutrition for both you and your baby. You may need to adjust your vitamin supplementation, and your healthcare team will monitor for nutritional deficiencies that could impact fetal development. Most women who become pregnant after gastric bypass have healthy pregnancies and babies, but specialized care is essential.
Because gastric bypass alters how your body absorbs nutrients, lifelong vitamin and mineral supplementation is essential to prevent deficiencies. Your typical daily supplement regimen will include: a bariatric multivitamin (taken twice daily), calcium citrate with vitamin D (1,200-1,500mg daily, taken in divided doses), vitamin B12 (sublingual or injection), and iron (especially important for menstruating women). Some patients may also need additional vitamin D, thiamine, or other supplements based on their blood test results. Your MemorialCare team will provide specific recommendations tailored to your needs and will monitor your vitamin levels through regular blood tests (typically at 3 months, 6 months, 12 months, and annually thereafter). Taking these supplements as directed is crucial for maintaining your health and energy levels in the long term.
While gastric bypass is technically reversible, reversal is a complex procedure that's rarely recommended or performed. The surgery is designed to be permanent, and reversing it eliminates the benefits of weight loss and improvement in obesity-related health conditions. In very rare cases where serious complications occur that cannot be managed through other means, reversal might be considered. More commonly, if issues arise or if inadequate weight loss occurs, revision surgery might be an option to adjust the gastric pouch or intestinal connection rather than completely reversing the procedure. This is why thorough preoperative preparation and understanding the permanent nature of this commitment are so important before proceeding with surgery.
The timeline for returning to work depends on the nature of your job and your individual recovery. If you have a sedentary desk job, you may be able to return within 2-3 weeks after surgery. If your work involves physical labor, heavy lifting, or strenuous activity, you'll likely need 4-6 weeks or more before returning to full duties. Many patients choose to start with part-time hours or lighter duties and gradually increase as they feel stronger. It's important not to rush back too quickly, as your body needs time to heal and adjust to your new eating pattern. Discuss your specific work situation with your surgeon, who can provide personalized guidance and provide any necessary work restrictions or documentation for your employer.