Published on Jan. 6, 2026
How one woman’s quick thinking, bystander CPR, and expert cardiac care helped her husband survive sudden cardiac arrest.
Ernest and Della Lee were spending a warm afternoon with family, celebrating Mother’s Day early in the South Bay. Married for 10 years and expecting their first child, the couple was savoring the moment—sharing comfort food and laughter. But what started as a joyful gathering quickly turned into a life-threatening emergency that would test their strength and underscore the power of expert, compassionate care.
Ernest, 44 and typically active, noticed tightness in his chest after lunch. His tightness faded away, so he brushed it off. But when the discomfort returned hours later, he grew concerned. The couple decided to drop off their grandmother and head to urgent care. What happened next would change everything.
A Sudden Collapse on the Freeway
While driving north on the 710 freeway, Ernest suddenly lost consciousness. His foot pressed down on the accelerator as the car continued at full speed. Della, eight months pregnant, sat beside him in the passenger seat.
“I was talking to him, and suddenly he just went quiet,” Della recalled. “I looked over, and he was completely unresponsive.”
Springing into action, Della climbed over the center console and took control of the wheel, steering between cars while trying not to panic. She managed to exit the freeway, reach a nearby intersection, and press her foot to the brake pedal, bringing the car to a stop.
“It was like being in a movie,” she said. “I didn’t know where I exited—I just knew I had to stop the car without crashing.”
Della laid on the horn to get the attention of nearby drivers and called 911. Three cars pulled over. Two bystanders helped pull Ernest out of the car and immediately began CPR. Della, eight months pregnant and emotionally shaken, provided rescue breaths in between chest compressions.
“He was turning blue, but you could still hear him trying to breathe,” she remembered. “I was just focused on keeping him alive until help came.”
The Race to Save a Life
Paramedics arrived within minutes. Ernest’s heart was shocked three times in the ambulance as Della rode beside him. He was transported to the emergency department at MemorialCare Long Beach Medical Center. Upon arrival, Ernest was diagnosed with ventricular fibrillation arrest (V-fib)—a life-threatening, erratic heart rhythm. An electrocardiogram revealed a ST-elevation myocardial infarction (STEMI), a severe heart attack caused by a blocked artery.
Cardiologists rushed him to the MemorialCare Heart & Vascular Institute cardiac catheterization lab, where he went into cardiac arrest again. This time, the team initiated venoarterial extracorporeal membrane oxygenation (VA-ECMO), which is an advanced form of life support that temporarily takes over heart and lung function, giving the medical team time to stabilize him and treat the underlying cause.
“Long Beach Medical Center was recently named an Extracorporeal Cardiopulmonary Resuscitation (ECPR) Receiving Center, and we are one of just five facilities in Los Angeles County to provide this advanced cardiac arrest care,” says David Shavelle, M.D., medical director, adult cardiology & interventional lab, MemorialCare Heart & Vascular Institute at Long Beach Medical Center. “This new designation is expected to help improve survival rates for patients who suffer sudden cardiac arrest. In this case, ECPR helped us keep oxygen flowing throughout Ernest’s body while we restored his heart rhythm.”
ECPR is a vital, time-sensitive intervention that provides a crucial lifeline when conventional resuscitation fails. Long Beach Medical Center’s readiness and expertise in deploying this advanced therapy underscores the Heart & Vascular Institute’s leadership in high-acuity cardiac response.
Interventional cardiologists placed a stent in Ernest’s right coronary artery to restore blood flow, drained fluid from his right lung, and placed him in a medically induced coma to aid recovery before surgery.
A Family in Crisis, A Team That Cared
While Ernest was in surgery, Della was directed to wait in the MHVI waiting room. The care team quickly recognized how vulnerable she was—eight months pregnant, alone and terrified—and made sure she was never left unsupported.
“The nurses and doctors kept checking on me,” she said. “They saw how far along I was and how scared I was, and they made me feel like I wasn’t alone.”
Soon after, Della’s mother-in-law and sister-in-law joined her in the waiting area. As they waited in silence, Della overheard something that gave her hope.
“There were two other families there who told me they chose Long Beach Medical Center on purpose,” Della said. “They said the cardiac care here is incredible, and Long Beach Medical was their first choice. Hearing that gave me comfort, and I knew Ernest was in the best hands possible.”
A Doctor Who Went Above and Beyond
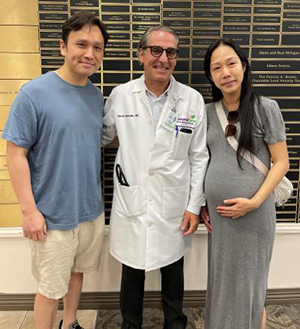
During Ernest’s stay, Dr. Shavelle made sure to be with both Ernest and Della every step of the way.
“Dr. Shavelle was there every single day,” Della said. “He hugged us, constantly checked in, explained everything in a way I could understand, and never made us feel like just another case.”
Even after Ernest’s discharge, Dr. Shavelle called personally to check in.
“Continuation of care is important, we always make sure our patients are doing well even after their discharged,” says Dr. Shavelle. “It’s always great to hear our patients are thriving after enduring a life-threatening condition.”
Ernest, though he remembers very little of his time in the hospital, clearly recalls a moment with Dr. Shavelle.
“I remember him hugging me and telling me, ‘Everything’s going to be okay,’” he said. “That meant everything.”
The Long Road Back—and Forward
After six days at Long Beach Medical Center, Ernest was stable enough to transfer to a local hospital for continued recovery. Today, he’s home and steadily healing. He still manages anemia and needs to stand slowly, but he walks 30 minutes a day on the treadmill and shows no signs of permanent damage.
“He’s doing great,” Della said. “He’s doing dishes, helping around the house, and walking fine. He has no neurological issues. It’s truly a miracle.”
This medical emergency significantly changed their lifestyle. Before this experience, Ernest and Della frequently ate out. Today, the couple prepares nearly every meal at home and focuses on heart-healthy habits. They approach life with a renewed sense of gratitude and purpose.
“We’re so grateful to everyone at the MemorialCare Heart & Vascular Institute at Long Beach Medical Center—this could’ve ended so differently,” said Della. “But because of the fast response, expert care, and the compassion we received, Ernest is here with us.”
Just weeks after Ernest’s discharge, Della gave birth to a healthy baby boy, bringing a joyful close to a chapter marked by resilience and love. The arrival of their child was a powerful reminder of everything they had overcome and everything they now had to look forward to.
Advice for Others
Della hopes their story encourages others to take even mild symptoms seriously.
“Don’t ignore things like chest tightness or dizziness,” she said. “Even if you’re young or think you’re in good shape, just message your doctor or use telehealth. That one small step could save your life.”
She also encourages families to seek care at trusted centers like Long Beach Medical Center.
“I wish every hospital was like this one,” said Della “The doctors, nurses, the whole team—they didn’t just save my husband’s life. They held me together, too.”